POSTPARTUM HEMORRHAGE (PPH) – “TIME IS OF GREAT ESSENCE MANAGEMENT
Peripartum hemorrhage remains one of the main causes of maternal mortality for decades worldwide.
- A key element of the hemostatic management is the development of standard operating protocols combining surgical as well as medical and hemostatic treatments depending on the cause and severity of bleeding.
- The presentation comprises the significance of using newer uterotonics, tranexamic acid, blood products such as FFP platelets , PRBC .
- In addition :the significance of antenatal evaluation and preparedness, vigilant monitoring and quick decision making in dealing with obstetric haemorrhage goes a long way in reducing morbidity.
DISCUSSION:
- The three take away messages
- PPH is any bleeding >500ml on mean within 24hrs of birth .
- But it is recommended to be in individualized based on the antenatal risk factors and geographical factors the women belongs to .
- The first step of PPH is to recognize that.
PPH is not a diagnosis but it’s a clinical sign of an underlying condition that by itself requires diagnosis.
- Though not predicable the major morbidities and mortalities caused by PPH is entirely preventable only by Vigilant Monitoring of not only High Risk But Also Low Risk women and the swiftness and certainty of the team is the greatest predictor of the outcome .
STANDARD OPERATING PROTOCOL – (PPH)
- It is highly recommended that every obstetric department develop SOP adopted to its location ,infrastructure and logistics.
- SOP should clearly aim to identify PPH at the earliest ,have an escalating mode of management ,draft transfusion protocols checkout the short term and long term mobilities, derive strong consensus for high risk obstetrics.
SOP AT SNS HOSPITAL
| Assess Antenatal risk factors anemia / systemic inflammatory /past H/o PPH /GHT / Bleeding diathesis / BMI. |
| LOW RISK | HIGH RISK |
| Adeqvate IV access in early labour . | Assessing biochemical parameters during early labour in all high risk women . |
| Prophylactic uterotonics . | Cross matching samples. |
| AMTSL. | |
| Our hospital prefers – inj carbetocin (better shelf life )100ug in during delivery of baby . | Prior information to from blood bank. |
| Obstetrician and paramedical team on site. | |
| Experienced anesthetist on call. |
“TIME IS OF GREAT ESSENCE MANAGEMENT”
A difficult situation of antepartum and postpartum hemorrhage is an enormous source of stress for the team and the patient as well.
Here we highlight the two significant cases..
CASES-1
- 30years | G2P1L1 | Pre caesarean delivery | term /Anemia treated with iron sucrose antenatally / late onset severe preeclampsia ( diagnosed a week back ) / |admitted ( first visit ) on 14/05/2021 @ 8.00 Am with C/O bleeding P/V diagnosed —ABRUPTION with DI C – Grade IV (with IUD & HELLP ) UNDERWENT laparotomy AT 08.30 AM – intrauterine – dead fetus delivered and retroplacental clots-800gm removed / couvelaire uterus.
- Packed RBC and FFPS’AND Platelets transfused .
- Postoperatively Patient had central serous retinopathy managed conservatively with CT and opthal opinion


DISCUSSION –
- Early intervention in pre eclampsia would have prevented morbidities
- Pre eclampsia and anemia is a dreaded combination
- It takes just few hours for a pre eclampsia women to land up in HELLP / DIC /IUD – so a vigilant monitoring and stringent protocol is absolutely essential.
CASES-2
- G2P1L1 | Pre FTND |booked and immunised outside/ admitted in active phase of labour @ 03.15 pm ( second visit)with thick meconium ,labour progressed well deliverd safe @ 04.35 pm .
- Interestingly we found the OS closing within 5 mins of delivery without expulsion of placenta DURING THIRD PHASE OF LABOUR
- Patient taken up for vaginal exploration and manual removal of placenta under shout GA @ —The ends of placenta could not be reached, only the few cotyteledons were palpable on the left cornual end of the uterine cavity.
- Decieded for emergency laparotomy @_05.30 pm with high risk consent .



INTRAOP FINDINGS :
- BICORNUATE uterus with a communication -placenta in the left horn –at about 500ml of clots in the right horn.
DISCUSSION
- A previous normal delivery doesn’t necessarily rule out uterine anomalies
- All retained placentae need not be given 30 min separation time.
- Uterus is a wonder organ as always – in this case we saw the cavity closes as soon as its empty.
- Need not panic about the closing os – understanding the basic physiology would help in diagnosis.
- AS ALWAYS KNOWN- MANY UTERINE ANOMALIES ARE DIAGNOSED PERIPARTUM .
During Dec 2020 –Nov 2021 , we encountered eleven cases of postparatum hemorrhage
each with different etiology – constitutes incidence of 10% of deliveries .
SEVERITY CAUSES

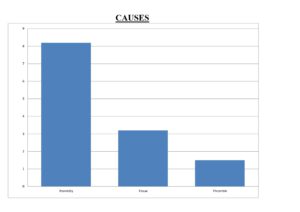
MAJOR PPH – 9 , MINOR PPH – 2 ATONICITY-9, TISSUE -1, THROMBIN -1
REQUIRING BLOOD PRODUCTS SURGICAL INTERVENTION


LAPAROTOMY-1 , MEDICAL MANGEMENT-10
ANTENATAL RISK FACTORS
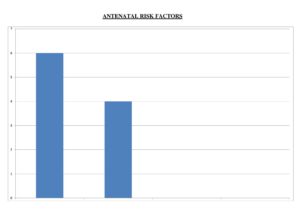
- ANTENATAL ANEMIA – 2 CASES
- SYSTEMIC INFLAMATION – 1 CASES
- SEVERE PRE ECLAMPSIA-2
- TWINS – 1CASES
- RISK FATORS -6 / NIL RISK- 5 CASES




